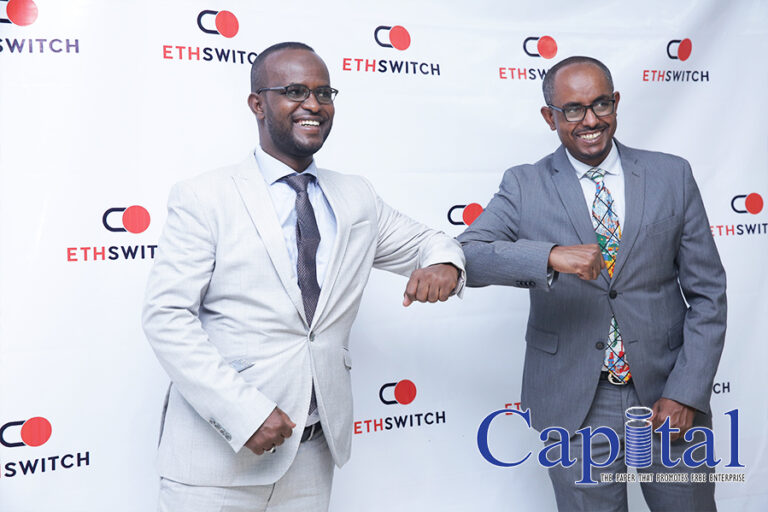
EthSwitch, a national switch, and Somali Microfinance Institution (SMFI) sealed a deal to include SMFI as the first micro financial firm to join EthSwitch as an indirect participant. The national payment solution is also introducing a national payment gateway.
EthSwitch which is the owner of Ethiopay, a domestic card scheme developed for all banks in Ethiopia to issue and acquire payment cards, has been working with all local banks for the last decade, while the coming of SMFI would be a new era for both the microfinance firm and the technology provider.
The statement that EthSwitch issued indicated that the participation enables Somali MFI to make its mobile wallet system interoperable with existing and upcoming payment systems allowing its customers to transfer funds to other financial institutions using their mobile wallet or accounts.
“The participation also enables Somali MFI to let its customers leverage payment acceptance devices deployed by banks and payment system operators across merchant locations,” it added.
So far banks are using the scheme on direct participation.
Yilebes Addis, CEO of EthSwitch, said that the e-payment solution is mainly undertaking three major goals including interoperability between financial firms, creating domestic payment scheme and infrastructure development for the use of financial firms.
“SMFI will benefit from the scheme that its customers shall easily issue cards to use payment terminals on banks and boost their existed mobile wallet service,” Yilebes explained.
Yilebes reminded that his company establishment targets to attain the national digital payments and financial inclusion strategies that banks, MFIs and as per the latest law payment system operators (ATM, POS, gateway, and switch operators) shall use it, “so it will ease the service of financial firms including the regional MFI.”
Khadar Ahmed, General Manager of SMFI, said that the institute is very strong regarding mobile money service and providing huge contribution for the society to ease the financial constrains.
“Switching our service with other financial firms will also expand the operation widely with positive accessibility for clients,” he said, adding, “The outreach for EthSwitch is also another contribution of the new deal.”
Including Somali MFI seven MFIs have bought share on EthSwitch, however, SMFI is the first to get approval from EthSwitch’s board of directors as an indirect participant after fulfilling the necessary requirements.
SMFI has bought the allocated 1035 shares of which 60 percent is paid. Through mobile transfer SMFI is facilitates 200 million birr daily transaction.
The membership also enables the microfinance institution to issue payment cards to its customers, which they can use on all of ATM and POS terminals.
Khadar told Capital that his institution is under preparation to issue cards to use the advantage and provide alternative for customers.
“We are the leader on the number of transaction under mobile money in the country and using cards is also more opportunity on the modern payment system,” he added.
“Under the piloting peer to peer (P2P) the microfinance will benefit more,” Yilebes explained. He explained that P2P is the new scheme which is under pilot stage is enable financial firms to transfer or pay money between each other’s besides the current service of using ATM and POS.
“An individual that have account on bank A shall pay for another person who have account on bank B without further process,” he explains about the new service “we have got positive results under the piloting and fully introduce in the coming financial year.”
For over five years EthSwitch has enabled to manage all ATMs under interoperable, and since last year using POS terminals operated by all banks.
Ethswitch, established in 2011, is a share company fully owned by all banks in Ethiopia. It is established mainly to provide simple, affordable, secured, and efficient e-payment infrastructure services to retail payment service providers, and through them, to end users in Ethiopia; by deploying technology.
Ethswitch is one of the two national switches in Africa that Yilebes says it has enable to cut unnecessary charges that may be occurred if the country uses foreign payment systems for its domestic payment solution.
The CEO explained that over 26.5 million numbers of transactions that have 28 percent increment compared with the preceding year have registered, while ATM cash withdrawal takes the 80 percent.
“POS interoperable has registered significant performance despite being new. In terms of profit it achieved 115 percent compared with the projection,” he added.
The CEO told Capital that it is on process and to some extent has tested to introduce a national and international payment gateway. The new scheme is targeted to facilitate payment through online for ecommerce transaction.
“We will provide a service for online payment gateway service providers not for customer or merchant,” he says “we are under implementation negotiation stage that would be available in the market to the maximum in six months, but if payment gateway licensed companies shall come in the short period we may commence the operation lesser than the given period.”
EthSwitch subscribed capital is 900 million birr. It is expected to handle payment system operators and payment instrument issuers when they are getting a green light from NBE.
So far information indicated that about 12 system operators and four issuers are on the pipeline to be operational as per the NBE directive that was issued recently under the way to financial inclusion and digital payment strategy.
EthSwitch and SMFI strike deal on payment solutions
New bank in the horizon following merger
Somali Microfinance Institution (SMFI) jointly with the under formation interest free banking (IFB), filed this week its application to the National Bank of Ethiopia (NBE) to evolve itself to become a bank under the brand name Shebele Bank.
SMFI which was established in January 2011 announced that it has agreed with the under formation IFB that is handled by the Somali community to narrow the gap to access to finance under Sharia law in the region. The moves come as the firms want to move forward to establish a single financial firm.
Khadar Ahmed, General Manager of SMFI, told Capital that they are going to file the application to NBE to allow them to upgrade into a bank as per the directives that was issued recently and under the minimum paid-up capital requirement directive that NBE reviewed couple of weeks ago.
In his recent interview with Capital Mustefe Mohammed, Vice President of Somali region, told Capital the regional administration is working with investors to invest in the region that has massive potential. Since then there were activities to establish banks under the initiative of investors in the region.
“There was a process to form a financial firm called Shebele Bank, while when NBE allowed MFI to grow to banks we had discussed with the founder of Shebele and agreed to work together and establish a single financial firm under the IFB scheme,” Khadar said.

He explained that, in the initial meeting that was held in the capital of Somali region, Jigjiga, NBE had participated in the event. “Since we have developed the required documentation, the corresponding documents will be filed for application and consideration to the NBE,” Khadar remarked.
As per the agreement, the new bank that is the result of SMFI and Shebele will be called by the name of Shebele.
SMFI has already met the requirement of minimum paid up capital of half a billion birr to establish a bank, Khadar says, adding, “Our capital of SMFI is 508 million birr and at the same time we are selling share for the public to amass more.”
SMFI under Sharia compliant has provided financial service in Somali region and other places like Dire Dawa and Addis Ababa city administrations. It has registered extraordinary achievement on mobile banking that is power by Bel Cash.
“We are confident that our hello cash mobile money service is the leading in the country since we have 750,000 users from urban to rural transactions since 2015,” Khadar explained.
As per the deal Bel Cash will transfer the technology and service for the financial firm in the near future.
In a directive issued August last year, NBE has allowed microfinance institutions to upgrade into full-fledged banks. So far Amhara Credit and Saving Institution have upgraded to become a bank under the name of Tsedey Bank.
Under the revised directive of NBE for banks minimum capital requirement that was issued in the second week of April, the newly coming Shebele Bank would fulfill its minimum paid up capital to 5 billion birr in seven years time.
SMFI has reached over one million of the public and of that 80 percent are active clients. The total amount of loan it provided is over 2.2 billion birr.
Under its mobile money service over 200 million birr per day is transacted on its platform. 19,000 point of sales and 42 branches have been managed by its services.
As of April 30, 2021, the total amount of outstanding loan is over 1.8 billion birr.
In a related development Oromia Credit and Saving Share Company will hold its first meeting on Monday May 24, to upgrade the Credit and Saving company to a full-fledged banking service.
Ascent capital caps $100 million in funds
Ascent Capital, a Kenya-based private equity manager has raised more than USD 100 million to its Ascent Rift Valley Fund to invest in small and medium enterprises in East Africa, surpassing the firm’s initial goal of USD 80 million.
ARVF targets small and medium-sized enterprises (SMEs) in Eastern Africa, looking to take large minority or majority stakes. The fund will provide funding to scalable SME businesses, helping to drive wider business and industrial development, particularly targeting the financial services, manufacturing, wholesale and retail trade and services, education, healthcare, and agro-processing sectors.
Ascent, which was among several new private equity firms established in the past decade to take advantage of growing popularity of the asset class in the region, had raised USD 80 million in its first round in 2015.
Ascent Capital was founded in 2012 and established its first fund, ARVF I, in 2014. Placements from ARVF I ranged from USD 2 million to USD 15 million, serving companies in Ethiopia, Uganda and Kenya. Ascent Capital is targeting a final close of ARVF II in December 2021 with a total volume of USD 120 million. The firm plans to invest from this fund in amounts of USD 4 million to USD 15 million, reaching SMEs in Ethiopia, Kenya, Rwanda, Tanzania and Uganda.
Dashen eases remittance via Silicon Valley partnership
Dashen Bank and Moneta Technologies, Ethiopia’s largest mobile Digital Wallet platform, partnered with the Silicon Valley, San Francisco based technology giant Flutterwave to up lift the traditional and expensive money transfer with modern platform for free of charge.
Africa’s leading payments Technology Company Flutterwave partnership with one of the leading financial firm in Ethiopia has expanded its activity to 34 countries in the continent.
The partnership that was announced on Tuesday May 20 allows facilitation of money transfer into Ethiopia through Amole, to Amole Wallet, bank accounts and cash pickup locations at over 2,500 locations across the country.
Asfaw Alemu, President of Dashen Bank explained that the new partnership with Flutterwave will serve the Ethiopian economy by making diaspora remittances easier for over 8 Million members of the Ethiopian Diaspora that remit over USD 5 billion annually to Ethiopia.
The statement of Dashen Bank said that international money transfer operators (IMTOs) and businesses on Flutterwave as well as Barter by Flutterwave users can send money into Ethiopia via this partnership.
It added that the remittance service in Ethiopia today is seen by users to be expensive, with manual paperwork and delays making it challenging and time consuming for the diaspora community. This partnership solves these problems by providing instant delivery of funds to the receiver at no fee, with more control of where and how to send money, including transparency from a regulatory standpoint.
Asfaw said that the new service has core value for the country’s economy and enables to boost the legal transfer and cut unnecessary costs the receiver or sender spend on the traditional money transfer.
Yemiru Chanyalew, CEO Moneta Technologies, said that the service provided by Flutterwave application through Amole may take very few seconds and the diaspora shall transfer the money for their beloved one from anywhere just by using the apps without visiting parallel banks or money transfer agents.
“The opportunity we have created with Flutterwave is the consumer has 100 percent control,” he says, adding, “we are very excited to work with Flutterwave and leverage our combined technologies to broaden our offering to the Ethiopian Diaspora community, our customers and merchants to enable cross-border remittance and commerce. At Amole, we are increasingly focused on cashless and eCommerce payments. Our combined efforts in enabling seamless and interoperable remittance and eCommerce payments will drive much desired financial inclusion in Ethiopia,” he said.
Asfaw told Capital that the all the deal with Flutterwave before the launch has been scrutinized by National Bank of Ethiopia, which is the financial sector regulatory body. “Flutterwave is a well-known company on the business and so far they have facilitated USD 9 billion. It is also working with 290,000 business community or companies through their platform,” he added.
 He said that the new scheme definitely would bring change on the money transfer and the forex generation for the country, “as a bank it saves the financial firm from other investments to compete with others since we avail such technologies that shall access the foreign currency from the source with providing modern technology.”
He said that the new scheme definitely would bring change on the money transfer and the forex generation for the country, “as a bank it saves the financial firm from other investments to compete with others since we avail such technologies that shall access the foreign currency from the source with providing modern technology.”
Flutterwave, which has key advantage on international payment processing in 150 countries and multiple modes including local and international cards, mobile wallets, bank transfer, and Barter by Flutterwave, has processed over 140 million transactions worth over USD 9 billion and it serves companies like Uber, Flywire, Booking.com and other prominent companies.